Is buprenorphine treatment just switching one addiction for another?
NO. With successful buprenorphine treatment as part of a complete treatment plan including counseling, the patient can put the addictive behavior into remission. Buprenorphine will maintain some of the preexisting physical dependence, but that is easily managed medically and eventually resolved with a slow taper off of the buprenorphine when the patient is ready. Physical dependence, unlike addiction, is not a dangerous medical condition that requires treatment.
Addiction is damaging and life-threatening, while physical dependence is an inconvenience, and is normal physiology for anyone taking large doses of opioids for an extended period of time. It is essential to understand the definition of addiction and know how it differs from physical dependence or tolerance.
When a patient switches from an addictive opioid to successful buprenorphine treatment, the addictive behavior often stops. In part due to buprenorphine's long duration of action, patients do not have physical cravings prior to taking their daily dose. The drug seeking behavior ends. Patients; regain control over drug use, compulsive use ends, they are no longer using despite harm, and many patients report no cravings. Thus all of the hallmarks of addiction disappear with successful buprenorphine treatment. Therefore, one is not trading one addiction for another addiction. They have traded a life threatening situation (addiction) for a daily inconvenience of needing to take a pill (physical dependence), as some would a vitamin. Yes the physical dependence to opioids still remains, but that is vast improvement over addiction, is not life threatening, and it can easily be managed medically.. Addiction is a brain disease that affects behavior. This addictive behavior can be devastating to the patient and their loved ones. It's not the need to take a medication that is the problem, many people need to take a medication, but rather it is the compulsive addictive behavior to keep taking it despite doing harm to one's self or loved ones that needs to stop. Whether or not the person takes a medication to help achieve this shouldn't matter to anyone. If a medication helps stop the damaging addictive behavior, then that is successful treatment and not switching one addiction for another.
What is difference between,physical dependence, tolerance and addiction?
The American Academy of Pain Medicine (AAPM), American Pain Society (APS), American Society of Addiction Medicine (ASAM), and NAABT recognizes these definitions below as the current accepted definitions.
I. Addiction: Addiction is a primary, chronic, neurobiologic disease, with genetic, psychosocial, and environmental factors influencing its development and manifestations. It is characterized by behaviors that include one or more of the following: impaired control over drug use, compulsive use, continued use despite harm, and craving.
II. Physical Dependence: Physical dependence is a state of adaptation that is manifested by a drug class specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug, and/or administration of an antagonist.
III. Tolerance: Tolerance is a state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more of the drug's effects over time. Physical dependence and tolerance are normal physiology. Addiction is a disorder that is damaging and requires treatment.
What is addiction?
To understand fully you must be aware of the difference between tolerance, physical dependence, and addiction: As a person takes opioids for an extended period of time, they become less sensitive to it and require more to achieve the same effect. Receptors in the brain become less sensitive. This means they need more and more opioid to achieve the same effect. This is called tolerance. When the body can no longer make enough natural opioids to satisfy the less sensitive receptors, the body becomes dependent on the external source. This is physical dependence. "Physical Dependence" is a physiological state of adaptation to a substance, the absence of which produces symptoms and signs of withdrawal. It is possible to be physically dependent on a drug without being addicted to it. Physical dependence is the result of physical changes in the brain. It is not a matter of willpower rather it is actual physiology. Addiction is defined as a behavioral syndrome characterized by the repeated, compulsive seeking (psychological dependence) or use of a substance despite adverse social, psychological, and/or physical consequences, along with the physical need for an increased amount of a substance as time goes on to achieve the same desired effect. Addiction is often (but not always, as with an addiction to gambling) accompanied by tolerance, physical dependence, and withdrawal syndrome. People are dependent on water and food but are not addicted to them. If a cancer patient is taking large doses of painkillers, he/she will become tolerant and physically dependent on them (meaning they will experience withdrawal symptoms if the drug is abruptly removed) but they are not necessarily addicted to it (meaning they will not seek out the drug despite adverse consequences once the drug is no longer needed for pain). Addiction is a disorder that requires treatment while physical dependence is not. This is important to understand in order to be able to discern between switching one addiction for another and treatment. The American Academy of Pain Medicine, American Pain Society, and American Society of Addiction Medicine, recognizes these definitions below as the current accepted definitions. I. Addiction: Addiction is a primary, chronic, neurobiologic disease, with genetic, psychosocial, and environmental factors influencing its development and manifestations. It is characterized by behaviors that include one or more of the following: impaired control over drug use, compulsive use, continued use despite harm, and craving. II. Physical Dependence: Physical dependence is a state of adaptation that is manifested by a drug class specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug, and/or administration of an antagonist. III. Tolerance: Tolerance is a state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more of the drug's effects over time. Summary: Addiction is uncontrollable compulsive behavior caused by alterations of parts of the brain from repeated exposure to high euphoric responses.
What is withdrawal?
Withdrawal syndrome consists of a predictable group of signs and symptoms resulting from abrupt removal of, or a rapid decrease in the regular dosage of, a psychoactive substance. The syndrome is often characterized by over activity of the physiological functions that were suppressed by the drug and/or depression of the functions that were stimulated by the drug. In other words, opposite of what the drug did. If the drug suppressed depression then the person would be depressed while in withdrawal. If the substance suppressed pain then the person will experience pain while in withdrawal. Withdrawal from opioids can be severe and excruciating. Withdrawal generally begins between 4 to 72 hours after the last opioid use (depending on dose and opioid), The symptoms are both physical and emotional and include: dilated pupils, goose bumps, watery eyes, runny nose, yawning, loss of appetite, tremors, panic, chills, nausea, vomiting, muscle cramps, insomnia, stomach cramps, diarrhea, shaking, chills or profuse sweating, depression, irritability, jitters, and increased sensitivity to pain. Withdrawal is a symptom of brain adaptations caused by some substances. As someone takes more and more of an opioid they increase their tolerance and require more and more to achieve the same effect. The level of tolerance where the body can no longer naturally compensate for the absence of the substance is called physical dependence. Withdrawal is a symptom of physical dependence. If you are not physically dependent on a substance you will not experience withdrawal from it. To achieve a comfortable transition off a medication you have become physically dependent on requires matching your taper off of the drug with your brain's ability to adapt to each decrease. Too fast will cause discomfort.
Is my medical information confidential?
Confidentiality of Alcohol and Drug Dependence Patient Records (summary) The confidentiality of alcohol and drug dependence patient records maintained by a practice/program are protected by federal law and regulations. Generally, the practice/program may not say to a person outside the practice/program that a patient attends the practice/program, or disclose any information identifying a patient as being alcohol or drug dependent unless: The patient consents in writing; The disclosure is allowed by a court order, or The disclosure is made to medical personnel in a medical emergency or to qualified personnel for research, audit, or practice/program evaluation. Violation of the federal law and regulations by a practice/program is a crime. Suspected violations may be reported to appropriate authorities in accordance with federal regulations. Federal law and regulations do not protect any information about a crime committed by a patient either at the practice/program or against any person who works for the practice/program or about any threat to commit such a crime. Federal laws and regulations do not protect any information about suspected child abuse or neglect from being reported under state law to appropriate state or local authorities.
Your Health Information Privacy Rights Fact Sheet:
THE CONFIDENTIALITY OF ALCOHOL AND DRUG ABUSE PATIENT RECORDS REGULATION AND THE H.I.P.A.A. PRIVACY RULE: SAMHSA
Code of Federal Regulations Title 42 Part 2 (42 CFR Part 2)
patient privacy
H.I.P.A.A. Website
What is buprenorphine or Suboxone?
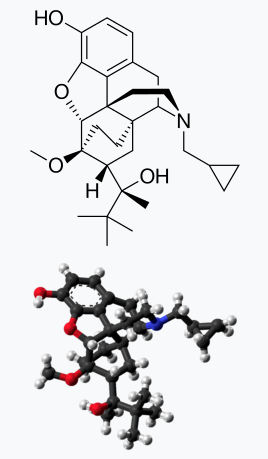
Buprenorphine (BYOO-pre-NOR-feen) is an opioid medication used to treat opioid addiction in the privacy of a physician's office.1 Buprenorphine can be dispensed for take home use, by prescription.1 This in addition to buprenorphine's pharmacological and safety profile makes it an attractive treatment for patients addicted to opioids.2 Buprenorphine is different from other opioids in that it is a partial opioid agonist3. This property of buprenorphine may allow for; less euphoria and physical dependence*3 lower potential for misuse*3 a ceiling on opioid effects*3 relatively mild withdrawal profile*3 At the appropriate dose buprenorphine treatment may: Suppress symptoms of opioid withdrawal2 Decrease cravings for opioids2 Reduce illicit opioid use2 Block the effects of other opioids2 Help patients stay in treatment2 * When compared with full opioid agonists (such as oxycodone and heroin)3 Buprenorphine ('bu-pre-'nôr-fen) (C29H41NO4) is a semi-synthetic opioid derived from thebaine, an alkaloid of the poppy Papaver somniferum. Buprenorphine is an opioid partial agonist. This means that, although Buprenorphine is an opioid, and thus can produce typical opioid effects and side effects such as euphoria and respiratory depression, its maximal effects are less than those of full agonists like heroin and methadone. At low doses Buprenorphine produces sufficient agonist effect to enable opioid-addicted individuals to discontinue the misuse of opioids without experiencing withdrawal symptoms. The agonist effects of Buprenorphine increase linearly with increasing doses of the drug until it reaches a plateau and no longer continues to increase with further increases in dosage. This is called the "ceiling effect." Thus, Buprenorphine carries a lower risk of abuse, addiction, and side effects compared to full opioid agonists. In fact, Buprenorphine can actually block the effects of full opioid agonists and can precipitate withdrawal symptoms if administered to an opioid-addicted individual while a full agonist is in the bloodstream. This is the result of the high affinity Buprenorphine has to the opioid receptors. The affinity refers to the strength of attraction and likelihood of a substance to bind with the opioid receptors. Buprenorphine has a higher affinity than other opioids and as such will compete for the receptor and win. It will "knock off" other opioids and occupy that receptor blocking other opioids from attaching to it. If there is enough Buprenorphine to knock the opioids off the receptors but not enough to occupy and satisfy the receptors, withdrawal symptoms can occur; in which case the treatment is more Buprenorphine until withdrawal symptoms disappear. In October 2002, the Food and Drug Administration (FDA) approved Subutex® (buprenorphine hydrochloride) and Suboxone® tablets (buprenorphine hydrochloride and naloxone hydrochloride) for the treatment of opiate dependence. These are the only buprenorphine based products approved to treat opioid dependence (addiction). On October 9, 2009 the FDA approved a generic version of Subutex. Suboxone, contains both buprenorphine and the opiate antagonist naloxone. Naloxone has been added to Suboxone to guard against intravenous abuse of buprenorphine by individuals physically dependent on opiates. If misused by injection, the naloxone will cause immediate withdrawal in opioid dependent people, however when taken sublingually, as indicated, the naloxone is clinically insignificant.
How buprenorphine works -- Graphics (PDF)
NAABT buprenorphine treatment brochure
buprenorphine-research